Latest News
 PHOTOS: Cleaning up Memorial Park
PHOTOS: Cleaning up Memorial Park
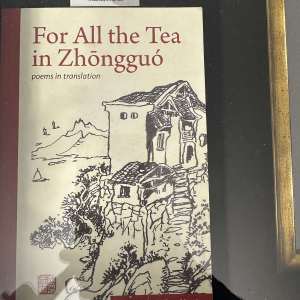 Martin discusses experience in China
Martin discusses experience in China

Harris Center conducts veterans hike at Jack’s Pond in Hancock
A group of veterans from around the Monadnock region, led by Susie Spikol of the Harris Center for Environmental Education, learned the little-known history of Hancock’s Jack’s Pond Sunday as part of the Harris Center’s veterans hiking program.The...

Mark Fernald’s maple syrup named best for third time in Ledger-Transcript contest
Mark Fernald of Sharon took home his second consecutive win and third overall among the judges at the Monadnock Ledger-Transcript’s 42nd annual maple syrup contest Saturday.The event was held at the Bantam Grill in Peterborough, where attendees had...
Sports
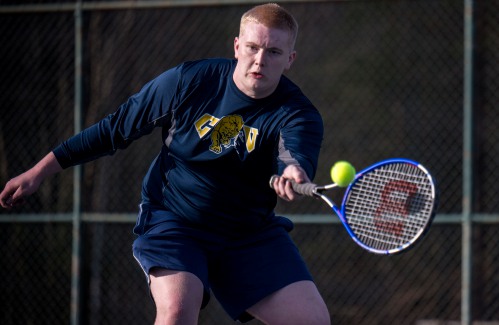
ConVal boys’ tennis looks to build experience
The ConVal boys’ tennis team comes into the season with almost no experience and a lot of work to do, but coach Mike Young relishes the challenge of building a full roster of players from the ground up. “You’ve got to start from the basics, which...
Opinion
Letter: Ban is not a political issue
Jeremy Margolis' article (“Senate OKs trans women sports ban,” April 9) struck me and, as a woman, I bristled.The article begins, "In the latest victory for Republicans… ." Why must this be presented politically? What has happened to humanity? This is...
 Margaret Nelson: View From the River – The gift of volunteers
Margaret Nelson: View From the River – The gift of volunteers
Business

Deb Caplan builds a business out of her creative passion
When she moved from Florida to New Hampshire in 2011, Deb Caplan, a lifelong creative, was thrilled to find that her new hometown of Peterborough was a major hub for for creativity and the arts in the Monadnock region.“I love living around here. There...
 Parker and Sons Coffee Roasting in Peterborough strives to create the perfect coffee
Parker and Sons Coffee Roasting in Peterborough strives to create the perfect coffee
 Happy Hardware looks to put the fun in hardware shopping
Happy Hardware looks to put the fun in hardware shopping
 Old Homestead Farm proposes short-stay cabins to supplement event business
Old Homestead Farm proposes short-stay cabins to supplement event business
Arts & Life

DubHub April art show features Loy and Andrews
dublinDubHub hosting April art showIn April, the Dublin Community Center, 1123 Main St. will feature the works of artists Eva-Lynn (“Evie”) Loy and Daniel Andrews, both of whom reside in Keene.A public reception is scheduled for Friday, April 12, from...
 Optimist Café to display Barbara Danser paintings
Optimist Café to display Barbara Danser paintings
 ‘Puppet’ tells Antrim native Dan Hurlin’s story
‘Puppet’ tells Antrim native Dan Hurlin’s story
 Exhibition on Screen features Sargent
Exhibition on Screen features Sargent
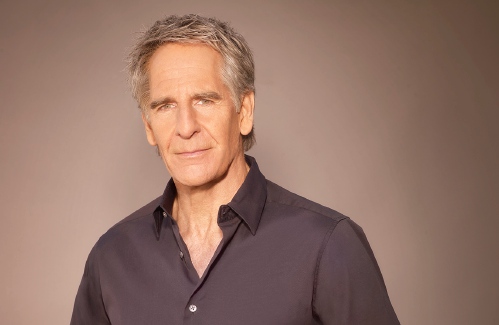 Scott Bakula starring in Peterborough Players’ ‘Man of La Mancha’
Scott Bakula starring in Peterborough Players’ ‘Man of La Mancha’
Obituaries
 Katherine W. Allen
Katherine W. Allen
Francestown NH - Katherine W. Allen of Francestown, NH and most recently of Hailey, Idaho died peacefully on February 16, 2024 at the age of 94. Born April 26, 1929 she was the daughter of ... remainder of obit for Katherine W. Allen
 Kenneth Noyd
Kenneth Noyd
Bath, ME - Kenneth Herbert Noyd was born November 27, 1930 in Norwood, Massachusetts. Ken passed away on April 7, 2024 at the age of 93 near Bath, Maine, after enjoying heartfelt conversati... remainder of obit for Kenneth Noyd
 Karen B. Ayers
Karen B. Ayers
, 80 Jaffrey, NH - Karen Backstrom Ayers of Jaffrey, NH, passed away in Keene, NH, on April 12, 2024. Karen was born on September 9, 1943, in Pittsburgh, PA, a daughter to Melvin Leslie and ... remainder of obit for Karen B. Ayers
 Donald Engelbert
Donald Engelbert
Sandown NH - Donald Craig Engelbert, 74, of Sandown, NH died on December 11, 2023, at his home surrounded by his family, accepting that cancer treatments were no longer beneficial and there... remainder of obit for Donald Engelbert

 Jack Kidd and Kidd Gloves make donation to Mt. Monadnock Little League
Jack Kidd and Kidd Gloves make donation to Mt. Monadnock Little League
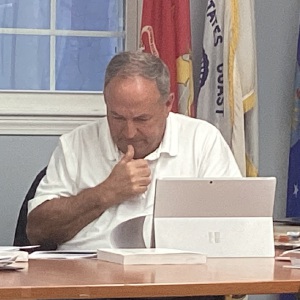 Old Homestead Farm in New Ipswich requests variance for short-term rental cabins
Old Homestead Farm in New Ipswich requests variance for short-term rental cabins
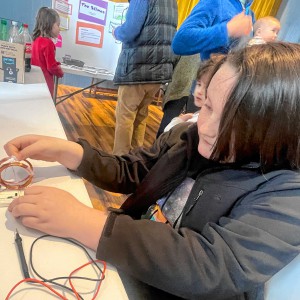 Young scientists show off their stuff at science fair in Francestown
Young scientists show off their stuff at science fair in Francestown
 Peterborough Farmers’ Market opens for the season
Peterborough Farmers’ Market opens for the season
 New Ipswich Congregational Church celebrates paying off mortgage
New Ipswich Congregational Church celebrates paying off mortgage
 HIGH SCHOOL SPORTS ROUNDUP: Tasha MacNeil leads the way for ConVal at Pelham Invita
HIGH SCHOOL SPORTS ROUNDUP: Tasha MacNeil leads the way for ConVal at Pelham Invita
 Grey Horse Candle Company opens Peterborough storefront
Grey Horse Candle Company opens Peterborough storefront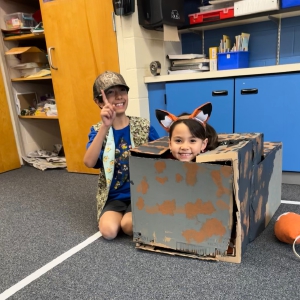 JGS Destination Imagination teams participate in regionals
JGS Destination Imagination teams participate in regionals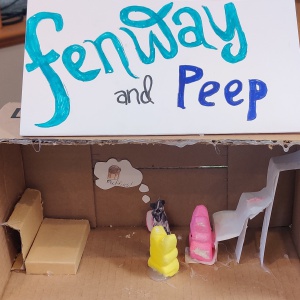 Hancock Town Library’s Literary Peep Diorama contest draws most-ever entrants
Hancock Town Library’s Literary Peep Diorama contest draws most-ever entrants Construction of joint Peterborough/Jaffrey water facility over 50% complete
Construction of joint Peterborough/Jaffrey water facility over 50% complete
 Monadnock Valley Patriots compete in state Special Olympics basketball tournament
Monadnock Valley Patriots compete in state Special Olympics basketball tournament Jed and Summer Bentley excel at Nordic skiing championships
Jed and Summer Bentley excel at Nordic skiing championships Marty Gitlin to present “The Ultimate Red Sox Nation” April 15 at Chamberlin Free Public Library in Greenville
Marty Gitlin to present “The Ultimate Red Sox Nation” April 15 at Chamberlin Free Public Library in Greenville
