Latest News
 ConVal attorney answers withdrawal questions
ConVal attorney answers withdrawal questions

Jaffrey kicks off Earth Week with no-waste potluck and environmental speakers
There were no paper plates or plastic utensils to be seen during the Jaffrey Climate Initiative and Jaffrey Conservation Commission Earth Day kickoff potluck on Tuesday, where participants were asked to bring their own plates and utensils for a...

Harris Center conducts veterans hike at Jack’s Pond in Hancock
A group of veterans from around the Monadnock region, led by Susie Spikol of the Harris Center for Environmental Education, learned the little-known history of Hancock’s Jack’s Pond Sunday as part of the Harris Center’s veterans hiking program.The...
Sports

Conant girls’ tennis continues to seek improvement
When Gloria Morison wakes up in the middle of the night, her mind turns to tennis.That's a good thing for her Conant girls' tennis team, as they can benefit from her late-night musings. Before Tuesday's home showdown with visiting Kearsarge, it was...
 Jack Kidd and Kidd Gloves make donation to Mt. Monadnock Little League
Jack Kidd and Kidd Gloves make donation to Mt. Monadnock Little League
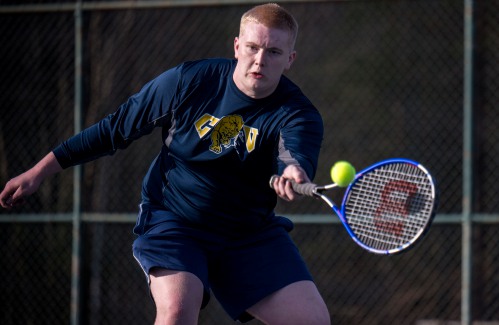 ConVal boys’ tennis looks to build experience
ConVal boys’ tennis looks to build experience
Opinion
Letter: Ban is not a political issue
Jeremy Margolis' article (“Senate OKs trans women sports ban,” April 9) struck me and, as a woman, I bristled.The article begins, "In the latest victory for Republicans… ." Why must this be presented politically? What has happened to humanity? This is...
 Margaret Nelson: View From the River – The gift of volunteers
Margaret Nelson: View From the River – The gift of volunteers
Business

Deb Caplan builds a business out of her creative passion
When she moved from Florida to New Hampshire in 2011, Deb Caplan, a lifelong creative, was thrilled to find that her new hometown of Peterborough was a major hub for for creativity and the arts in the Monadnock region.“I love living around here. There...
 Parker and Sons Coffee Roasting in Peterborough strives to create the perfect coffee
Parker and Sons Coffee Roasting in Peterborough strives to create the perfect coffee
 Happy Hardware looks to put the fun in hardware shopping
Happy Hardware looks to put the fun in hardware shopping
 Grey Horse Candle Company opens Peterborough storefront
Grey Horse Candle Company opens Peterborough storefront
Arts & Life
Gnome Notes: Emerson Sistare – Amor Towles weaves tapestry in ‘Table for Two: Fictions’
A book review by The Toadstool Bookshop in Peterborough.“Table for Two: Fictions,” by Amor TowlesWhile some authors have name-recognition, others have “title-recognition” -- when one or more their works is so widely read that it has overshadowed its...
 Jaffrey Civic Center hosting Heart of the Arts
Jaffrey Civic Center hosting Heart of the Arts
 Project Shakespeare to present ‘The Miraculous Journey of Edward Tulane’
Project Shakespeare to present ‘The Miraculous Journey of Edward Tulane’
 The Thing in the Spring returns May 16
The Thing in the Spring returns May 16
 Project Shakespeare seeks summer students
Project Shakespeare seeks summer students
Obituaries
 Bonnie Paquette
Bonnie Paquette
Bennington, NH - Bonnie (Adams) Paquette, 65, of Bennington NH, passed away on April 13th, 2024, at Concord Hospital, surrounded by her family. The daughter of Ruth Greeley and Robert Adams... remainder of obit for Bonnie Paquette
 Katherine W. Allen
Katherine W. Allen
Francestown NH - Katherine W. Allen of Francestown, NH and most recently of Hailey, Idaho died peacefully on February 16, 2024 at the age of 94. Born April 26, 1929 she was the daughter of ... remainder of obit for Katherine W. Allen
 Kenneth Noyd
Kenneth Noyd
Bath, ME - Kenneth Herbert Noyd was born November 27, 1930 in Norwood, Massachusetts. Ken passed away on April 7, 2024 at the age of 93 near Bath, Maine, after enjoying heartfelt conversati... remainder of obit for Kenneth Noyd
 Karen B. Ayers
Karen B. Ayers
, 80 Jaffrey, NH - Karen Backstrom Ayers of Jaffrey, NH, passed away in Keene, NH, on April 12, 2024. Karen was born on September 9, 1943, in Pittsburgh, PA, a daughter to Melvin Leslie and ... remainder of obit for Karen B. Ayers

 Peterborough Planning Board approves 14-unit development near High Street
Peterborough Planning Board approves 14-unit development near High Street
 Franklin Pierce students help foster literacy at Rindge Memorial School
Franklin Pierce students help foster literacy at Rindge Memorial School
 Peterborough firefighters continue fishing derby tradition
Peterborough firefighters continue fishing derby tradition
 HOUSE AND HOME: The Old Parsonage in Antrim is a ‘happy house’
HOUSE AND HOME: The Old Parsonage in Antrim is a ‘happy house’ Former home of The Folkway in Peterborough is on the market
Former home of The Folkway in Peterborough is on the market Two Jaffrey-Rindge Destination Imagination teams move on to Globals
Two Jaffrey-Rindge Destination Imagination teams move on to Globals Parker and Sons Coffee Roasting in Peterborough strives to create the perfect coffee
Parker and Sons Coffee Roasting in Peterborough strives to create the perfect coffee
 HIGH SCHOOL SPORTS ROUNDUP: Tasha MacNeil leads the way for ConVal at Pelham Invita
HIGH SCHOOL SPORTS ROUNDUP: Tasha MacNeil leads the way for ConVal at Pelham Invita
